
Science
What is the Retina?
At Vision Care Group, we challenge ourselves to think of all the ways we can improve the lives of the visually impaired. As the world population continues to age, particularly in countries like Japan, retinal diseases are expected to become an increasingly prevalent cause of visual impairments. Our subsidiaries, VCGT Inc. and VCCT Inc., are committed to developing treatments for these retinal diseases.
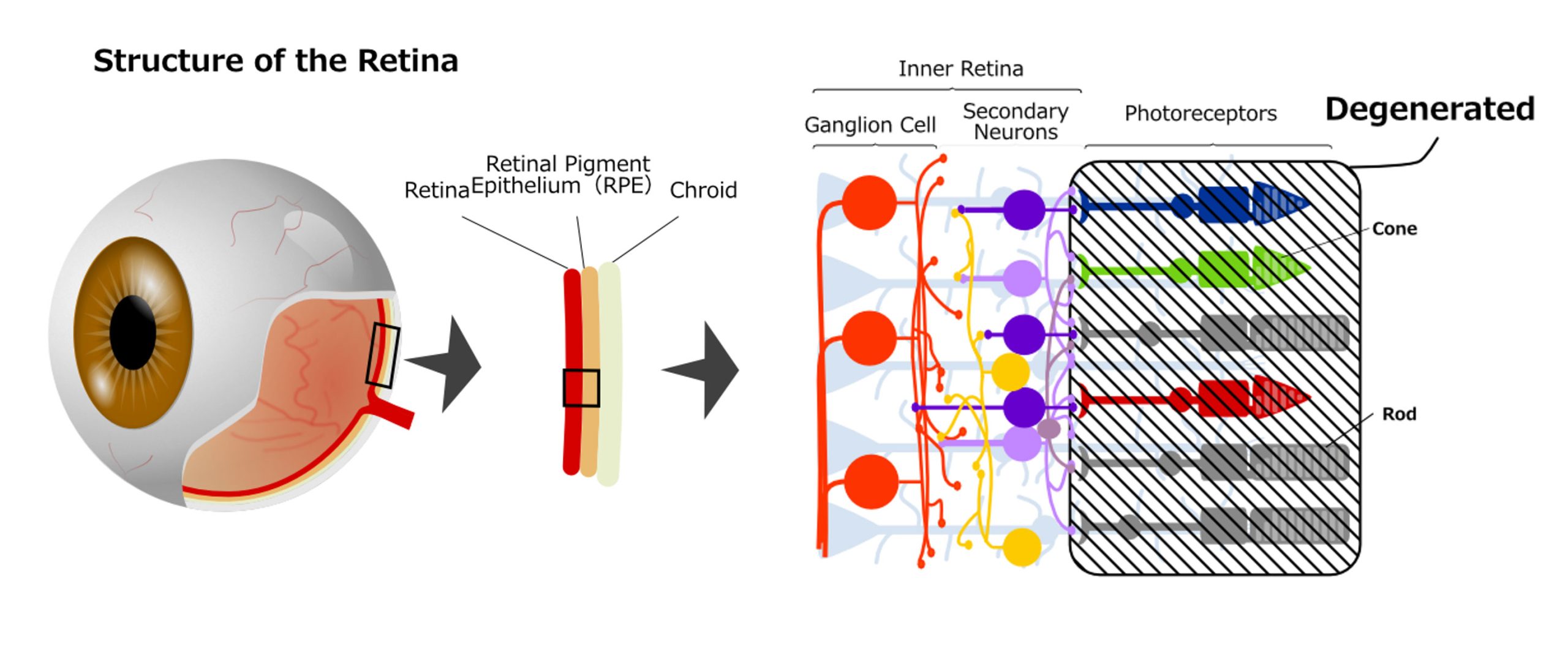
The retina, a nerve tissue located at the back of the eyeball, plays a critical role in vision. Light first passes through various transparent tissues, including the cornea, lens, and vitreous, before it reaches the retina. Here, the light is absorbed by specialized photoreceptor cells. This light information undergoes preliminary processing within the retina before it is transmitted to the brain. The retina consists of layers of distinct cells as follows from the outside:
- Retinal Pigment Epithelium (RPE) layer: This is a layer of special epithelial-like tissue derived from the same neural tube as the sensory retina, which plays a variety of roles including maintaining photoreceptor cells.
- Photoreceptor cell layer: Named for their distinctive cellular shapes, this layer is composed of two types of photoreceptor cells, rod cells and cone cells, each equipped with specialized cell compartments for light sensing. Rod cells, which mediate vision in dim light conditions, are broadly distributed across the retina. Conversely, cone cells, responsible for color and high-resolution vision, are primarily concentrated in a specialized area known as the macula.
- Secondary nerve layer: Contains bipolar cells, which are second-order neurons. Horizontal cells and amacrine cells process signals from photoreceptor cells and send them to the next layer.
- Retinal G4. ganglion Cell (RGC) layer: Ganglion cells in this layer have long projections that form the optic nerve and transmit encoded visual information to the brain.
Cell Therapy (Regenerative Medicine)
Cell therapy serves two primary purposes. One is to harness the ‘trophic effect,’ where nutrients produced by stem cells help suppress inflammation in tissue and promote regeneration. Mesenchymal stem cells often produce this effect, and therapies using these cells are typically administered intravenously. The second purpose is to replace damaged cells and reconstruct tissue. In this case, surgery is required to replace the local cells. Unlike traditional treatments with small molecules or protein antibodies, cell therapy is a surgical procedure that uses live cells as a material. The effectiveness of this treatment is largely influenced by the patient’s microenvironment, as the cells can change according to the condition of the patient’s tissue.
The retina is a part of the central nervous system, formed during early development as an outpocketing of the central portion of the brain. It is a crucial component of the visual system, and damage or disease can cause visual impairment. However, since retinal cells do not regenerate, the only way to reconstruct the tissue is through regenerative medicine (cell therapy).
Basic research has shown that fetal retina, ciliary body cells, and Müller cells have the potential to produce retinal cells. However, currently, cell transplantation materials primarily use fetal retina, embryonic stem (ES) cells, and induced pluripotent (iPS) cells. We were the first to report primate ES cell-derived retinal pigment epithelial cells and their potential for therapeutic use. Subsequently, after the emergence of iPS cells, we made significant strides toward its clinical application.
Gene Therapy
Retinal degeneration diseases refer to diseases causing degeneration of photoreceptor cells. Except for age-related macular degeneration (AMD) that occurs in the elderly, they are all genetic disorders. Inherited Retinal Diseases (IRD) can be caused by genetic mutations in the photoreceptor cells or in the Retinal Pigment Epithelium (RPE). Over 200 causal genes have been identified, with inheritance patterns including autosomal dominant, autosomal recessive, and X-linked recessive. Regardless of the specific genetic circumstance, the fundamental approach to treatment invariably lies in gene therapy targeting the causative gene.
The retina is second only to cancer in terms of the extensive application of gene therapy. Several strategies are currently under clinical trials: a) supplementing genes of nutrient factors (trophic factors) for photoreceptor cells, b) causal gene therapy (b1: supplementing the correct gene, b2: editing the causal genetic mutation via genome editing), and c) optogenetics, which allows cells other than photoreceptor cells to respond to light. Among these, the possibility for a curative treatment lies primarily in the category of cause-specific gene therapies, the most famous of which is the RPE65 gene therapy. Unlike the RPE65 gene therapy, which has demonstrated some restorative effects through enzyme gene supplementation, the majority of gene therapies aim not at restoring function but at preserving existing function. It is also worth noting that these treatments are often most effective when administered early, with effectiveness often decreasing the longer treatment is delayed.
AI in medicine
The development of AI has led to the early development of AI-based image diagnosis software in the field of ophthalmology, especially for retinal diseases. The success rate of diagnosis is already impressive, and it is anticipated that AI will eventually bring about substantial transformations in the field of ophthalmology. Progressing further, our aim is to incorporate the comprehensive knowledge and expertise our group of ophthalmology clinicians have gathered over the years into an AI software. This includes our experience in diagnosing and treating retinal degenerative diseases, genetic diagnosis, explaining diseases and their prognosis, determining the suitability of regenerative medicine and gene therapy, low-vision care, as well as giving advice on lifestyle and life planning. Through this AI integration, we hope to ensure accurate advice can be widely disseminated around the world.
Other
We are also branching into other areas with the goal to provide total solutions for the visually impaired. For example, we are actively working on automatic driving and advanced driving support systems for people with visual field impairment. Our newly established driving consultation clinic in Kobe Eye Center for visually impaired people has been well received. We are preparing to implement these initiatives with the aim of widespread adoption of our expertise in using driving simulators and providing driving consultations. The ultimate goal is to enable ophthalmology practices everywhere to provide driving advice for people with visual impairments. We are also working on the implementation of multiplex PCR testing for determining the causes of ocular infections, real-time immune rejection detection testing for retinal cell transplantation, and the development of ophthalmic surgical robots.
